Disc Herniation in the Lumbar Spine
If you are between the ages of 20-50 and have acute onset of low back pain, you may have a lumbar disc injury, a common problem for people in this age group.
The first thing to understand about the spine is that our structure has a purpose, and our lifestyle can have a negative impact on our structural integrity. We were not designed to sit for long periods of time. Indigenous societies did not regularly use chairs; they would primarily squat, which keeps the spine in a neutral position. As a sitting society, the incidence of back pain is at record highs, for reasons I will explain.
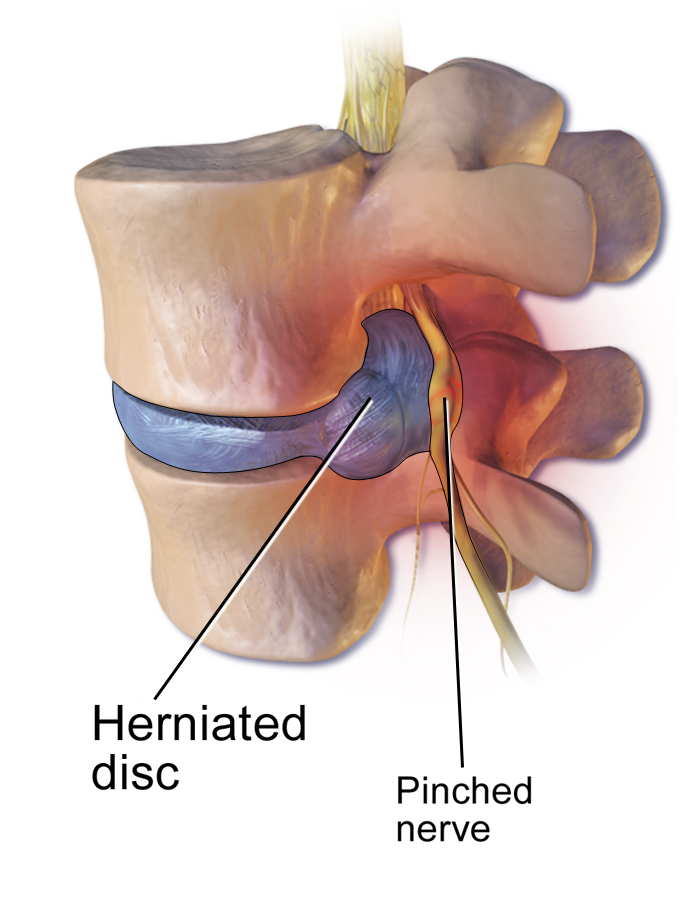
Our spine has 3 primary curves, seen from the side: The neck (cervical spine) curves in, the mid-back (thoracic spine) curves out and the low back (lumbar spine) curves in again. These curves are important for shock absorption and allow for optimal movement of each spinal segment. Since our topic relates to the lumbar spine, you should know that lumbar lordosis, the gentle curve inwards, is important to attain and maintain for disc health and optimal function. Without lordosis, there is excessive pressure on the front of the disc, causing the material inside the disc to slowly migrate posteriorly, which can result in a protrusion. This happens over time, and pain may begin slowly, but a telltale sign of disc herniation particularly if you are in this age group is your back “gives out”, followed by severe pain that may be localized or radiating into one or both of your legs. This can happen any time during the day, but since disc material attracts water, your discs, including any herniations present, are at their largest in the morning.
This is why we frequently hear of the acute onset of pain when someone bends over to put on their socks, for example. Generally speaking, this is not a problematic activity but is simply the last straw for your back. If you have spent extended periods of time sitting, particularly with your lumbar spine flat or slumped, then you are in prime condition for experiencing this unpleasant problem. The disc material can slowly move back far enough to where the posterior disc wall fails, resulting in severe pain.
How to manage this problem:
First, let’s talk about what not to do. Do not try to “stretch it out”. The muscles of your back will feel tight, because they are contracting to protect your injured spine. You may therefore feel like you should bend forward to stretch them. This however, will push more disc material towards the rear of the disc and perpetuate and possibly worsen the problem. Slumping may make it feel better, because you are opening up the posterior disc space, giving the protrusion more space and thus alleviating some of the pressure from the protrusion. However, this can also perpetuate and possibly worsen the problem for the same reason you should avoid stretching.
So, what should you do?
Unfortunately, I have disc pathology. This began, ironically, in PT school from sitting for 16 hours a day on a regular basis. Experience is a great teacher, and I learned a lot about disc healing that has hopefully benefitted others as well. The following is a summation of recommendations based on my work with patients for over 25 years as well as extensive education, and research.
Is it an emergency?
You should go to the ER if you are experiencing any of the following:
• Muscle weakness, such as you are unable to lift up your foot or your leg gives out when you try to walk.
• Loss of control of bowel or bladder function.
• Pain of such severity that you are unable to move and care for yourself.
Fortunately, those occurrences are not the norm. Most people experiencing this problem will benefit from the following:
At the time of injury:
• If you are able to take over the counter anti-inflammatories, this can help significantly.
• Lie down for a few hours, preferably on ice. Rather than just lying back on your bed, sit on the side of the bed, lie down on your side and then roll back onto your back.
After several hours or if you are unable to lie down:
• Avoid sitting. If you are unable to avoid sitting, try to self-traction in a chair by pushing down on the armrests and unweighting your lower body as much as possible.
• Walk, but just slowly and around your home.
• When standing try to self- traction by pushing down on a counter top to unweight your spine and lower body. Traction creates a negative pressure in the disc, which can help reduce the herniation, but it may be painful initially because of the inflammatory response. Keep it gentle.
• Lie down frequently if possible.
• Call your physical therapist. While you have a bit of a road to travel for healing, some interventions can help such as myofascial release, laser, electrical stimulation, kinesiotaping, and gentle traction.
For the next 6-8 weeks: Even if you feel better before this, just know that you are at high risk of re-herniation because it takes this amount of time at a minimum to heal soft tissue. You should attempt to create the optimal environment for reducing the herniation and promoting healing. Many people unknowingly contribute to the scenario where the disc remains herniated, and thus they remain in chronic pain or in need of surgery. The most important things to do during this phase are:
• Keep your spine in neutral and in particular DO NOT BEND FORWARD!!! – Flexion avoidance for at least 6 weeks in critical in order to help the disc protrusion to reduce in size and to allow the posterior wall of the disc to heal well.
• Minimize lifting – If possible, do not lift anything over 10 lbs; if you must, be sure to lift with your legs, keeping your spine in a neutral position, maintaining the lordosis.
• Traction – This may be painful initially because of the inflammation around the disc, but after the acute phase, separating the segments of the lumbar spine can create a negative pressure in the disc, which may help it to reduce. Traction in prone (on your stomach) or in supine (on your back) with legs straight is ideal because you want the normal lumbar lordosis to be present. Motorized or manual traction is offered in many clinics. Home devices are also available, such as the Saunders® lumbar home traction device, an inversion table with quick release at the knees (don’t use this option if you have high blood pressure), or functional traction belts, that you can use in sitting and standing, such as the DDS 300 by Disc Disease Solutions, Inc.
• Repetitive movement – Most disc herniations occur in a posterior or posterolateral direction (towards the back of the disc). In this case, the most effective movement for facilitating the reduction of the disc is extension (arching your back). Just like pressure on the front of the disc, as with slumping, likely caused the problem in the first place, placing pressure towards the back of the disc can help move the disc material back into place. This is best done under the supervision and advice of a physical therapist, because If you extend too far too soon, you could approximate the sides of the vertebrae, leaving a portion of the disc outside. Initially, extension may be no more than just creating a normal neutral arch in your back. Do not push into pain. This is a slow-moving structure that you will try to modify over time.
• TENS (transcutaneous electrical neuromuscular stimulation) – This is an electrotherapeutic modality that you can purchase and use at home for pain management. These devices are widely accessible, and can be used as needed to manage pain. The idea is that by stimulating the receptors for touch, the transmission of the pain signal to the brain is interrupted at the level of the spinal cord. If you are a good responder to TENS, this can be very helpful for pain management during the acute phase of healing.
• Physical Therapy – Many Physical Therapists are experts in the management of spinal disorders, and can be very helpful in guiding you through your healing, utilizing techniques that will help shorten the duration of pain, and hopefully prevent the next episode. An approach that is particularly helpful for management of disc disorders is the McKenzie method. Therapists trained in this approach can determine the appropriate direction, amplitude, and dosage of repetitive movement that will be most helpful in promoting the reduction of the disc.
Please note that this article in no way replaces the need for medical advice regarding your own situation, but rather is intended as a general overview for a common problem. Unfortunately, there are many types of dysfunctions that can occur in the spine, so please see a medical practitioner for assessment when needed. And also note that a “no pain, no gain” philosophy is not applicable to back problems. Any activity that hurts, even if it is supposedly good for your back, should be avoided. Wishing you a happy back!